The debate over COVID-19 treatments has resulted in the emergence of “forced prescribing and dispensing” laws that are under consideration in many states.
These laws would require physicians to prescribe any treatment the patient wants and pharmacists to dispense the medication regardless of clinical appropriateness.
What Is Driving These Laws
Supporters of these bills are motivated by patients feeling a need to be more involved in their treatment protocols and a desire to increase access to unproven COVID-19 therapies such as ivermectin, hydroxychloroquine (HCQ), and chloroquine (CQ).
Nearly eight in 10 Americans believe or are unsure about at least one common falsehood regarding COVID-19 or the vaccines.1 At least 37 bills in 16 states have drafted legislation to promote use of off-label COVID-19 therapies.
Study Methods
The study was conducted between October 15, 2019 and February 15, 2020. It included adult patients with a history of asthma or COPD admitted to one of the SAHS hospitals with an order placed for ipratropium/albuterol, fluticasone/salmeterol, mometasone/formoterol, or budesonide/formoterol MDIs. Patients who were presumed to have or tested positive for COVID-19 were excluded from the study.
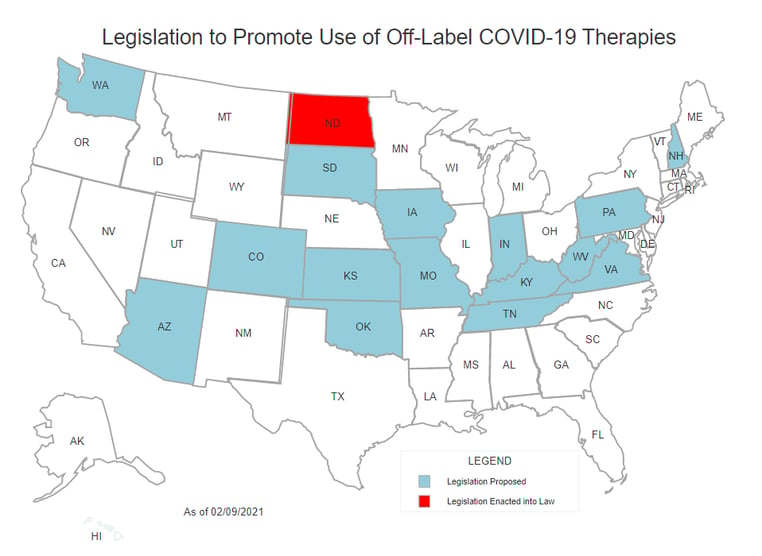
Source: ASHP
Common Components of Off-label COVID-19 Bills
These bills typically prohibit prescribers from declining to prescribe treatments to patients who request them and prohibit pharmacists from declining to dispense or even question those prescriptions.
Further, these bills prohibit licensing boards from investigating or taking disciplinary action against licensees that provide off-label treatments and put in place standing order/non-prescription access to off-label treatments.
While some of these bills apply only to specific medications — most commonly ivermectin, hydroxychloroquine (HCQ), and chloroquine (CQ) — some apply to any medication prescribed off-label for treatment of COVID-19, even in the presence of an absolute contraindication. While the bills often strip important safety guardrails performed by the pharmacist, some of the proposed legislation still holds the pharmacist liable for adverse events from the medication.
Key Points from Advance Bills
These proposed bills eliminate pharmacists’ clinical judgement regarding dispensing off-label use of unproven therapies and dictate that pharmacists may not refuse to fill certain prescriptions for any reason. If passed, consequences for violating these laws include monetary fines, loss of license, and/or criminal charges.
These bills can progress rapidly in state legislatures. Fervent supporters of these bills take measures to silence opposing viewpoints and stifle open debate. However, more extreme measures such as forced dispensing and prescribing can potentially be softened through negotiation.
Advocacy Tips
As healthcare professionals, what can we do to prevent or slow these bills from becoming law?
- Get involved and actively monitor bills related to off-label use of COVID-19 therapies in your state
- Monitor activity and be prepared to submit written testimony prior to a hearing
- Mobilize your colleagues to advocate for the profession through:
- Attending committee hearings
- Writing and sending letters to state representatives
- Work with other pharmacy, hospital, and provider organizations in your state to establish a unified front against forced prescribing and dispensing bills
Conflicts Presented by These Bills
Existing law already permits prescribing and dispensing of off-label treatments. Though off-label prescribing is not confined to certain drugs and indications, any practitioner can claim any prescribed drug is being utilized for off-label use. Forced dispensing laws are essentially unnecessary, but they functionally remove critically important safety functions provided by the pharmacist.
In addition, these bills threaten to damage public trust in pharmacists and healthcare professionals. Pharmacists could be forced into knowingly dispensing a medication that is likely to cause patient harm, and still remain liable for resulting patient injury.
Currently, all states have existing statutes confirming pharmacists’ ability to decline to fill a prescription based on clinical judgement and the patient’s best interest. Several states have “conscience” clauses that permit pharmacists to decline to fill certain prescriptions based on moral or ethical objections.
CPS Can Help
CPS can help support your organization and protect patients with TELEpharmacy solutions that monitor and communicate with patients post-release regarding their questions and concerns around their medication(s). CPS’ TELEpharmacy Solutions are proven to help reduce adverse drug events and costly hospital readmissions.
For more information, contact CPS:
1 KFF COVID-19 Vaccine Monitor (October 14-24, 2021).

 All Posts
All Posts